 An eating disorder can affect anyone at any age, any sport, any background and any gender. The symptoms may build slowly well before the illness becomes evident.
An eating disorder can affect anyone at any age, any sport, any background and any gender. The symptoms may build slowly well before the illness becomes evident.
Often it is an athletes support team such as parents, friends, team mates and coaches that pick up on the symptoms and can prevent the disorder from ruining the athletes sporting career.
The very characteristics that make a good athlete such as having an ‘A’ type personality, dedicated, focused, high achievers, perfectionist and self-critical are also the same traits found in those with eating disorders. Added to this, athletes keen to adopt food practices which enhance performance, appearance and health are more vulnerable to misinformation about nutrition.
Coaches need to be particularly aware of issues regarding body composition to ensure that athletes can differentiate between natural body weight, shape and size versus body fat. Care should be also be taken not to encourage athletes to compete in categories that are beyond their natural physique and capability.
If concerns arise, then seek professional help from a sports dietitian and doctor as soon as possible.
The athletes most affected
All athletes are at risk especially those who are involved in sports that focus on appearance and weight such as:
- Gymnasts, ballet dancers
- Jockeys
- Light weight rowers & coxswain
- Wrestlers, martial arts
- Runners
- Cross country skiers
- Cyclists
- Endurance athletes
Affects on performance
Long-term health risks
An athlete needs peak physical and mental health if they are to train and perform to their full potential.
Unfortunately eating disorders not only lead to reduced performance, but can also disturb relationships with family and friends. Time can be lost training and long-term health risks may develop such as: osteoporosis, infertility, stress fractures, recurrent illness, infection, fatigue, loss of concentration and mental stress.
Early intervention can reverse many of these factors.
Physical changes with falling BMI
Body mass index (weight kg/height m²) or BMI is commonly used to classify weight categorises in adults. A normal weight is 18.5-24.9. However as weight falls optimal performance suffers. Concern may be raised when BMI is within the range of 17.5-19. At this point athletic results during training and performance are reduced and an athlete shows the following signs of change:
- Women athletes experience irregular or absent period (amenorrhea)
- Decreased blood levels of iron and iron stores (ferritin)
- Stress fractures
- Poor heart performance
- Food or weight obsession
- Fatigue
- Vomiting
- Decreased VO2 Max
Alarm bells should ring when an athlete’s BMI falls below 17.5 as performance and training become impaired and the athlete may experience:
- Anemia
- Osteoporosis
- Collapse
- Death
| Symptoms of an eating disorder | |
|---|---|
| Reduced performance | Fatigue, low energy |
| Frequent injury | Mottled teeth |
| Loss of monthly period | Chest pain |
| Vomiting and purging | Depression, mood swings |
| Isolated eating habits | Risk of suicide |
| Distorted body image | Anxiety |
| Laxative use | Cold intolerance |
| Bingeing out of control eating | Bloated/heartburn |
| Stress fractures | Constipation |
| Infections | Diarrhoea |
| Preoccupation with food, shape and weight | Social withdrawal Guilt |
| Self esteem based on weight and shape | Highly self-critical Growth failure |
Why do eating disorders occur?
Eating disorders arise from a complex combination of (usually) long-term behavioural, emotional, psychological, inter-personal and social factors. Food may be used as a means of control to compensate for feelings and emotions that may seem overwhelming at the time. Some of the issues that may lead to eating disorders include:
Psychological Factors
Low self-esteem; feelings of inadequacy; depression; anxiety and loneliness.
Interpersonal Factors
Troubled family or close relationships; history of being teased about weight; difficulty expressing emotions and feelings and feelings of isolation within their peer group.
Social Factors
Cultural pressures which value thinness and body perfection rather than inner qualities and strengths.
Other Factors
Research is now focusing on the brain chemicals which control appetite, hunger and digestion to see if imbalances could be a contributing factor.
Different Types and Symptoms
Anorexia nervosa
Despite a dramatic loss in weight, the sufferer still feels fat; distorted body image; amenorrhea; obsession with exercise; mood swings and changes in personality and behaviour; low self-esteem; downy hair growth; laxative abuse and vomiting after use; avoidance of food-related social events such as eating with the family, keen to cook for others but not share in the meal.
Medical concerns: poor circulation and feeling excessively cold, fatigue, dizzy spells, swollen glands, digestive tract dysfunction, osteoporosis, sleep disturbances and more prone to infections.
Bulimia nervosa
Weight may not change despite over-eating followed by self-induced vomiting or
purging with laxatives and fasting. Characterised by secrecy, shame and guilt until help is sort. Large volumes of food consumed can make this an expensive habit; feelings of lack of control over eating behaviour; frequent trips to the toilet, especially after meals; depressive mood, personality and behaviour change.
Medical concerns: Damage to kidneys; Swollen glands; Damage to stomach and oesophagus; Loss of body fluids/dehydration; Muscle cramps and weakness; Fainting spells; Fits and irregular heart beats; Mottled teeth due to the effect of acid reflux on tooth enamel.
Compulsive eating (Binge Eating)
This is characterised by bouts of over-eating which are not always in response to hunger and can be secretive and embarrassing to the sufferer. The bingeing may follow a period of rigid dieting, setting up a yo-yo pattern of diet and bingeing. Binge eating is not usually related to purging, fasting or laxative abuse.
Medical concerns: Fluctuating weight levels; depression.
Muscular dysmorphism (Bigorexia)
This is typically found in body-building circles. It is a condition where sufferers are constantly worried about being too small. They worry that they are not lean or sufficiently muscular even when this is not the case. They may spend long hours lifting weights and obsessing about their diet often following extreme high-protein, very low or no-fat diets. Often socially isolated, they may suffer from depression and low self-esteem.
Medical concerns: Abuse of anabolic steroids or other body-building drugs and sporting supplements, such as creatine and protein powders. Kidney failure and loss of bone density may result.
Anorexia athletica (Compulsive exercising)
This is characterised by excessive exercising beyond that required for effective training and competition in order to compensate for food eaten. The fear of weight gain despite low body weight; Defining self-worth in terms of performance; stealing time from work, school or relationships to exercise; excessive restraint in the amounts and types of foods eaten.
Medical concerns: fatigue; amenorrhea; nutrient deficiency; loss of bone density, muscle cramps and weakness.
ED-NOS (Eating disorder not otherwise specified)
A catch-all phrase for eating disorders that don’t exactly fit the parameters of anorexia or bulimia. Food may be restricted but the person is not yet underweight; the female may be anorexic but still has menstrual periods; bingeing without purging; regularly chews food but spits it out without swallowing; obsessive about weighing their body several times a day.
Night-Eating Syndrome
Caught between anorexia in the morning and binge-eating all night. The sufferer may experience problems with falling asleep and/or staying asleep. Eating causes guilt and shame, feelings of tension and anxiety.
Helpful tips
If you suspect someone has an eating disorder;
- Be aware the person may not welcome your comments
- Avoid being seen as an accuser
- Express concern about their health and well-being
- Emphasise that you are on their side and want to encourage them to see a health professional
- It may help to focus on the symptoms they themselves are concerned about e.g.fatigue, loss of performance. Slow healing stress fractures.
- Agree to disagree about strongly held beliefs e.g whether they are under weight or not.
- Allow time for them to consider your comments rather than expecting an immediate response.
- If they are ambivalent about getting help focus on them having an assessment first rather than accepting treatment.
- Ask what you can do to help.
Treatment Pathway
Eating disorders are best treated by a group approach involving the following key groups:
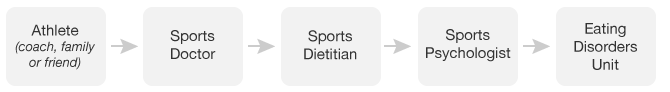
If you are concerned about your own eating or someone close to you then don’t delay, contact us and your doctor as soon as possible.























































Leave a Reply